Abstract
Nocardia is an opportunistic pathogen that most frequently affects the lungs. Evidence is limited regarding the risk factors for nocardiosis. The current study assessed clinical correlates of nocardiosis. A retrospective study was conducted based on medical records of consecutive adult patients (N = 60) with nocardiosis hospitalized during 2007–2018 at a tertiary hospital in central Israel. A matched comparison group of 120 patients was randomly selected among hospitalized patients with community-acquired pneumonia. Multivariable conditional logistic regression models were fitted. Immunosuppressive pharmacotherapy was positively associated with nocardiosis (matched odds ratio [OR] 4.40, 95% confidence interval [CI] 2.25–8.62, p < 0.001), particularly corticosteroid therapy (matched OR 4.69, 95% CI 2.45–8.99, p < 0.001). Systemic corticosteroid therapy was strongly associated with pulmonary nocardiosis (matched OR 5.90, 95% CI 2.75–12.66, p < 0.001). The positive association between solid organ transplantation and nocardiosis was attenuated following adjustment for systemic corticosteroids in a multivariable model. The association between corticosteroid therapy and nocardiosis appeared stronger in patients with chronic pulmonary disease (OR 5.74, 95% CI 2.75–12.66, p < 0.001) than in the pooled analysis of all nocardiosis cases. In conclusion, corticosteroid therapy was strongly correlated with nocardiosis, particularly among individuals with chronic pulmonary disease and in pulmonary nocardiosis.
Similar content being viewed by others
Introduction
Nocardiosis is an opportunistic infection that typically occurs in individuals with a history of solid organ transplantation (SOT)1, malignancy2, human immunodeficiency virus infection3 or chronic pulmonary diseases4. Evidence on the independent contribution of each of these conditions to nocardiosis risk remains limited, since most studies were case-series and lacked a comparison group. It is also unclear if the likelihood of nocardiosis is related to the underlying disease itself or to the immunosuppression therapy administered against it.
Corticosteroid therapy is prevalent amongst individuals diagnosed with nocardiosis5,6. A European multicenter case–control study conducted among SOT recipients (SOTR) showed that corticosteroid dosage was related to the risk of nocardiosis (odds ratio [OR] 1.12, 95% confidence interval [CI] 1.03–1.22 for each milligram increase in corticosteroid dose), and a strong positive association was found between high calcineurin inhibitor and nocardiosis (OR 6.11, 95% CI 2.58–14.51)1. As corticosteroid therapy is the standard of care for many conditions that might be also associated with nocardiosis, such as SOT, chronic pulmonary diseases and cancer, the independent role of each factor, warrant further investigation.
As Nocardia is mostly transmitted by inhalation or aspiration7, the lungs are the primary site of infection in more than two-thirds of the nocardiosis cases3. However, evidence on the risk factors for nocardiosis, beyond the general propensity to develop bacterial pneumonia, remains unknown.
The current study aimed to assess clinical correlates of nocardiosis, and was designed to identify their contribution to the development of nocardiosis, beyond the risk of pneumonia requiring hospitalization.
Methods
Study design and population
A retrospective study was conducted based on the medical records of patients aged 18 years or older who were hospitalized during 2007–2018 at Rabin Medical Center (RMC), a tertiary hospital in central region of Israel. All citizens in Israel have health insurance, according to the universal health insurance law implemented in Israel since 1995. Each citizen is insured by one of the four health maintenance organizations (HMOs) that provide primary/community health-care services and cover hospitalizations costs. The hospitalization records that were the main source of information in this study are linked to the medical records of the primary/community health care system run by the HMOs. This enabled comprehensive assessment of clinical and laboratory features of all the patients included in the study.
We reviewed the microbiology laboratory records for all the patients with Nocardia isolation during 2007–2018. Nocardia isolation was defined as the laboratory detection of Nocardia, sampled from an individual patient. We identified all consecutive patients with Nocardia isolation who received a formal diagnosis of nocardiosis by an infectious disease specialist, and who were treated accordingly. The exclusion criterion was Nocardia colonization. To ensure appropriate classification, an infectious disease specialist (EG) reviewed the medical charts of all the patients from whom Nocardia was isolated, and confirmed the diagnoses, as described elsewhere8.
A comparison (control) group included hospitalized patients with a clinical diagnosis of pneumonia during 2007–2018, who were identified by hospitalization diagnoses codes of the World Health Organization International Classification of Diseases 9th Revision (ICD-9)9 (see the list of diagnoses in the supplementary methods). The rationale behind the selection of a control group with pneumonia is that nocardiosis mostly affects the lungs, and we aimed to identify specific correlates of nocardiosis beyond the propensity of having a relatively frequent lung infection such as pneumonia. Accordingly, our approach of selecting hospitalized patients with pneumonia as a control group is intended to minimize the identification of non-specific correlates that might occur if a healthy control group was selected. Patients diagnosed with aspiration pneumonia were excluded from the study. Randomly selected 120 controls were individually matched to cases according to the year of diagnosis, in a ratio of two controls per case.
Data collection
Information on the study variables was abstracted from the medical records of the patients of both groups. If the records indicated repeated infections with Nocardia or repeated hospitalizations due to nocardiosis or pneumonia, only the first episode was included.
The main dependent variable was hospitalization due to laboratory-confirmed clinical nocardiosis (see definition of cases), coded as 1; or hospitalization due to pneumonia caused by other pathogens, coded as 0.
The independent variables included demographic and clinical characteristics, which were defined based on documentation in medical records. The demographic variables included: age at the year of index hospitalization, sex, and socioeconomic rank of town of residence (following the classification of the state Central Bureau of Statistics10). The clinical variables included: smoking status, basic physical function (bedridden or mobile), and background illnesses (e.g. cancer, organ transplantation). The Charlson comorbidity index was calculated11.
For the 90-day period prior to the diagnosis, data were collected on hospitalizations and pharmacotherapy, including immunosuppressive and immunomodulatory treatments. These treatments included systemic and topical corticosteroids, other immunomodulatory agents (e.g. methotrexate and azathioprine), anti-rejection immunosuppressants (e.g. calcineurin inhibitors, mTOR inhibitors and mycophenolate mofetil) and anti-cancer drugs (alkylating agents, antimetabolites, anti-microtubule agents, topoisomerase inhibitors and cytotoxic antibiotics). Data on Pneumocystis jirovecii prophylaxis with trimethoprim/sulfamethoxazole (TMP/SMX) were collected as well.
For systemic corticosteroids, the average daily dose during the 90 days prior to the index hospitalization was documented. To facilitate comparisons of dosage, for corticosteroids other than prednisone, the prednisone equivalent dose was calculated using the standard conversion factors12.
As secondary objectives, we examined differences between patients with nocardiosis and patients with pneumonia at time of hospital admission in results of tests. These included vital signs, complete blood count, C-reactive protein (CRP), and albumin levels, as well as in radiological findings. We also assessed the one-year mortality after admission. These data were also collected from the medical records.
The information retrieved from hospitalization files was crosschecked against the medical records of the primary care/community HMO system and patient prescription records.
Laboratory methods
During the study period, sputum, bronchoalveolar lavage, blood and tissue samples from infected individuals were incubated on blood and chocolate agar plates for 2–4 days. When Nocardia was suspected, samples were incubated also on Thayer–Martin agar plates for up to 14 days. Between 2007 and 2011, Nocardia identification was based on macroscopic evaluation accompanied by microscopic assessment for distinguishing features (e.g. pseudohyphae). These were confirmed by biochemical markers such as ortho-Nitrophenyl-β-galactoside and catalase. Since 2011, Nocardia was identified using matrix-assisted laser desorption/ionization time-of-flight mass spectrometer (MALDI-TOF), with a sensitivity of 95%.
Statistical methods
Demographic and clinical variables of the patients with nocardiosis (cases) and control group (pneumonia patients) were compared using bivariate and multivariable conditional logistic regression models. Correlations between the independent variables were assessed using Spearman’s rank correlation coefficient, and highly correlated variables (correlation coefficient > 0.6) were assessed in separate models. Independent variables were selected to be included in the multivariable model based on the bivariate analysis and on prior knowledge (i.e. associated with nocardiosis such as immunosuppression treatment1). Independent variables were excluded from the model if they were associated with nocardiosis with p > 0.2, and if they yielded a change of less than 10% in the point estimate of the association between immunosuppression treatments and nocardiosis (suggesting that they were not confounders13). Interactions between the independent variables were assessed in the models. Collinearity between the independent variables was assessed using variance inflation factor. Matched ORs (and 95% CIs) were obtained from the conditional logistic regression models. P < 0.05 was considered statistically significant. Correction for multiple comparisons was conducted using the Benjamini and Hochberg false discovery rate method14. Sensitivity analyses were conducted to explore possible sex and other clinical related differences. The chi square test was used to assess heterogeneity in the association measures between men and women.
Data analysis was undertaken using IBM SPSS version 23 (Armonk, New York, USA) and WinPepi15.
Ethical approval
The Helsinki committee of Rabin Medical Center approved the study protocol. An exempt from informed consent was given by the Helsinki committee of Rabin Medical Center due to the retrospective design of the study. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Results
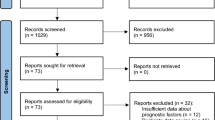
Between January 2007 and June 2018, Nocardia was isolated from 78 individuals treated at RMC. Of these, 18 were excluded due to either lack of sufficient data or the absence of clinical diagnosis of nocardiosis (Fig. 1). The number of patients with nocardiosis was distributed similarly along the study period (supplementary Table S1).
The majority of the patients with nocardiosis had an immunosuppressive condition (N = 45, 75%) (see the supplementary results for the list of immune suppressive agents). Of these, the most prominent conditions were SOT (N = 16, 27%) and malignancies (N = 10, 17%). Fifteen (25%) patients had a chronic pulmonary disease, two thirds of them (N = 10) were treated with corticosteroids during the 90 days prior to the diagnosis of nocardiosis (Fig. 2).
Background illnesses of the 60 patients with nocardiosis. 1The patient had radiological findings suspicious for glioma but she refused a biopsy; 3Acute lymphoblastic leukemia (1), Acute myeloid leukemia (1), Chronic lymphocytic leukemia (1), Chronic myeloid leukemia (1); 4The patient was diagnosed with Nocardial endocarditis.
Nocardiosis most frequently involved the lungs (N = 48, 80%). In 39 (65%) patients the lungs were the sole organ involved. Brain imaging was performed for 47 (78%) of the individuals with nocardiosis, and the infection involved the central nervous system in 10 (17%) patients. The involvement of the skin and soft tissue was found in 9 (15%) patients. One patient had Nocardial endocarditis that involved a prosthetic heart valve.
Analysis of nocardiosis correlates
The mean age of patients with nocardiosis was 60.3 (15.6) years, compared to 73.8 (17.1) years in patients with pneumonia (p < 0.001). No significant differences were noted between the groups in sex distribution and socioeconomic status (p = 0.166 and p = 0.125, respectively) (Table 1).
Mean scores on the Charlson comorbidity index did not differ significantly between patients with nocardiosis and those with pneumonia (p = 0.125). The proportion of patients with SOTR was higher in the case than control group: 27% versus 3%, p < 0.001, while the proportion with solid malignancies was lower: 5% versus 17%, p = 0.084. A higher proportion in the nocardiosis group was hospitalized during the 90 days prior to the diagnosis of nocardiosis than the control group: 53% versus 33%, p = 0.037.
Compared to those with pneumonia, the patients with nocardiosis were more often treated with immunosuppressive and other immunosuppression conferring agents (i.e. immunomodulatory agents, anti-rejection immunosuppressants and anti-cancer drugs), and more often received prophylactic treatment with TMP/SMX (18% vs. 1%, p = 0.001), systemic immunosuppression agents (73% vs. 19%, p < 0.001) or more than one immunosuppressive agent (35% vs. 8%, p < 0.001). The use of corticosteroids was documented among 72% of patients with nocardiosis versus 13% of those with pneumonia (p < 0.001). Among individuals administered systemic corticosteroids, the dosage of corticosteroids did not differ significantly between the case and control groups (p = 0.850). The adjusted p values calculated for multiple comparisons yielded similar results.
Multivariable analysis
Before conducting a multivariable analysis, correlations between the independent variables were assessed. Mostly weak or non-statistically significant correlations were found.
A multivariable conditional logistic regression model that included all the patients with nocardiosis showed that pharmacotherapy with any immunosuppressive agent was strongly positively associated with nocardiosis: matched OR 4.40 (95% CI 2.25–8.62), p < 0.001. In this model, the inverse association between age and nocardiosis remained significant, while the associations of sex, Charlson comorbidity index, SOT and hospitalizations during the 90 days prior to nocardiosis were not statistically significant (Table 2).
Another model included treatment with corticosteroids as the main independent variable showed a strong positive association between treatment of corticosteroids and nocardiosis: matched OR 4.69 (95% CI 2.45–8.99), p < 0.001, while adjusting for the aforementioned confounders (Table 3).
Stratifying the analysis by sex showed a stronger association between treatment with corticosteroids and nocardiosis among males (matched OR 7.61 [95% CI 2.74–22.16, p < 0.001]) than among females (matched OR 3.29 [95% CI 1.27–8.52], p = 0.014) (Table 3); however, the chi square test for heterogeneity was not significant (chi square 1.35, p = 0.245). Limiting the analysis to patients with chronic pulmonary disease showed that the association between treatment with corticosteroids and nocardiosis might be stronger than in the general sample of nocardiosis patients: matched OR 5.74 (95% CI 1.92–17.15, p = 0.002), but the CIs were overlapping. Similar results were obtained when the analysis was limited to patients with pulmonary nocardiosis (Table 3).
The independent role of SOT in nocardiosis was evaluated in models that included SOT as the main independent variable. In this analysis, the positive association between SOT and nocardiosis was attenuated following adjustment for demographic and clinical factors, and became non-significant following adjustment to the dosage of consumed systemic corticosteroids (Table 4).
Radiological characteristics
The majority of patients with pulmonary nocardiosis (N = 48) had either solitary infiltrate (N = 17, 35%) or bilateral infiltrates (N = 11, 23%). Solitary nodule (N = 1, 2%) or multiple nodules (N = 5, 10%) were also observed, and 4 patients (8%) had both infiltrates and nodules. Additional 4 (8%) patients had a pulmonary abscess. Six (13%) patients had other radiographic presentations, such as pleural effusion or dissolution of the surgical anastomoses.
Among 111/120 (93%) of patients with pneumonia (control group), a pulmonary infiltrate was evident on chest radiogram on admission. Among the remaining nine individuals, pneumonia was diagnosed based on clinical signs and symptoms (i.e. fever, respiratory symptoms, elevated markers of inflammation and compatible auscultator findings). Bilateral diffuse pneumonia was evident in 14/111 (13%) of pneumonia controls, whereas single side pneumonia was evident in 97/111 (87%) of them.
Vital signs and blood parameters at admission
Among patients with nocardiosis, the mean saturation was significantly higher, and the proportion with dyspnea was lower, than among patients with pneumonia. The mean hemoglobin and albumin levels were significantly lower in patients with nocardiosis than in patients with pneumonia. No significant difference was found between the groups in CRP and in counts of white blood cells and platelets (Table 5).
Blood and sputum cultures from the control group (patients with pneumonia) were positive in 14/120 (12%), with Streptococcus pneumoniae being the leading pathogen (29%) isolated from the blood.
Overall survival
There was no significant difference in mortality one year after hospitalization between patients with nocardiosis and the pneumonia controls: 33% and 38% respectively, p = 0.623.
Discussion
We compared the correlates between patients with nocardiosis and hospitalized patients with pneumonia, thus enabling the assessment of clinical correlates of nocardiosis beyond the propensity to develop pulmonary bacterial infection in general.
The main finding of the current study is that treatment with any immunosuppressive agent and particularly with systemic corticosteroid therapy was strongly related to an increased risk for nocardiosis, independent of demographic characteristics and other recognized risk factors for nocardiosis. Our finding regarding the association between corticosteroid therapy and nocardiosis is similar to that reported by Coussement et al.1. In their multicenter study of SOTR, the OR for nocardiosis was 1.12 per each milligram of corticosteroids. In the current study, the association between corticosteroid therapy and nocardiosis surmounted the association between a history of SOT and nocardiosis. This suggests that the history of SOT is merely a mediator variable for corticosteroid therapy rather than an independent risk factor for nocardiosis. Indeed, when the use of systemic corticosteroid therapy was included in the regression model, the association between SOT and nocardiosis was not significant. Coussement et al.found that high through levels of calcineurin inhibitors increased the risk for nocardiosis substantially, compared with corticosteroid therapy. As there were only 16 (27%) SOTR in our cohort, statistical power was lacking to evaluate calcineurin inhibitor as a risk factor for nocardiosis amongst SOTR.
The point estimate for the measure of association of systemic corticosteroid therapy with nocardiosis was somewhat higher amongst individuals with chronic pulmonary disease than in the cohort as a whole. Nocardia is an intracellular bacteria16 and the host's immune reaction against infection broadly relies on macrophage activity17. In contrast to nocardiosis, pneumonia in hospitalized patients is usually caused by typical, extracellular bacteria18. Individuals with chronic pulmonary diseases were found to have a higher rate of macrophage dysfunction19. It is therefore assumed that the macrophage activity of individuals with chronic pulmonary diseases treated with corticosteroids is particularly decreased, exposing them to a higher risk for nocardiosis. Corticosteroid therapy particularly damages the alveolar macrophages20. This can explain the increased effect of such treatment on the risk of developing pulmonary nocardiosis.
Systemic corticosteroid therapy is known to increase the risk for respiratory infections in general, including pneumonia21,22. In the current study, the inclusion of patients with pneumonia was not restricted to those with isolated bacterial pathogens, and it is likely that some of the patients in the control group had viral pneumonia. However, in comparing patients in the nocardiosis and the control groups, we were able to distinguish correlates that were associated with nocardiosis relative to ordinary pneumonia.
Overall, 60 patients with clinically and laboratory-confirmed nocardiosis were identified for the 12-year period. Although different methods for identifying Nocardia were used in the earlier and later periods, the average yearly number of patients with nocardiosis did not differ significantly over the study period. We therefore assume that nocardiosis incidence at our center was not affected by diagnostics. Previous studies from two other tertiary hospitals in Israel reported 39–53 cases of nocardiosis during a similar time interval, about one decade ago23,24. The higher number of cases observed in our study might be due to differences in case definitions across the studies. However, it also might reflect an increase in the incidence of nocardiosis. Advances in medical technologies have led to an increased prevalence of individuals living with transplanted organs25 or with chronic pulmonary diseases26, thus might have resulted in a larger population susceptible to nocardiosis. RMC is a tertiary hospital in the central district of Israel. In addition to serving residents of the central district, RMC is a referral hospital that serves patients from around the country. Moreover, due to the additional tertiary hospitals in the region, the exact size of the population served by RMC cannot be estimated accurately. Accordingly, in the absence of a concrete denominator, we could not estimate the nocardiosis incidence rate. However, for a single center, the number of patients with nocardiosis in our series was higher than reported over a similar period in France27. This might be due to differences in patients' mix and case definitions.
While former reports showed that males comprised more than half the patients with nocardiosis1,27,28,29, males comprised only 48% of our patients with nocardiosis. We found no significant difference in the distribution of sex between the groups. However, the association between corticosteroid therapy and nocardiosis was stronger in males. Nonetheless, the heterogeneity test was not significant, likely due to the small sample size. An underestimation of the realistic effect of this interaction is possible, considering the lower adherence rates of males to pharmacotherapy in general30, and to immunomodulatory therapy in particular31. However, previous reports on the susceptibility to opportunistic infections in the setting of corticosteroid therapy did not show a difference between the sexes32,33. As corticosteroid use may reflect the severity of the underlying disease, the susceptibility of corticosteroid-treated males to nocardiosis may merely be a surrogate for their poorer physical condition, exposing them to nocardiosis. In our study, most of the chronic lung patients had either chronic obstructive pulmonary disease or bronchiectasis, diseases that require systemic corticosteroid therapy for acute exacerbations34,35, and which carry a poorer prognosis in males36,37. Further research is required to elucidate this issue.
The current study had several limitations, particularly the retrospective design. Differences in the recording of medical information might have existed between physicians; and the accuracy regarding some of the study variables, such as pharmacotherapy and dosages, might not be optimal. To increase the validity of the information retrieved from hospitalization files, data were crosschecked against other medical charts, such as the HMO systems and patients' prescription records. Medical data, such as physicians' prescriptions and medication purchasing are continuously and automatically recorded for all insured members. Thus, differential misclassification of the main study variables, such as immunosuppressive pharmacotherapy, is unlikely. Moreover, since the study sample comprised hospitalized patients with a relatively high comorbidity burden, such information bias, if existent, would likely be non-differential. Notably, since nocardiosis is a relatively rare infection, the total number of cases was too small to yield statistical power for assessing risk factors in specific sub-populations.
As a single center study, a selection bias should be considered. However, it is unlikely that patients with nocardiosis at RMC differ from patients diagnosed at other tertiary hospitals. Moreover, the selection of nocardiosis patients and control patients with pneumonia from the same hospital mitigates differences in referral patterns between the groups. As all patients with nocardiosis at RMC during the study period were included in the study, selection bias of the cases is unlikely. We combined all the patients with nocardiosis as one group, though their underlying diseases varied (as demonstrated by the inclusion of SOT and pemphigus). This approach might have led to the "dilution" of a given factor that specifically characterized a subgroup of patients. This limitation was dictated by the small number of patients with nocardiosis, and the even smaller numbers of important subgroups such as SOT. Consequently, addressing the effect of anticalcineurin inhibitor type or serum level on the risk of developing nocardiosis was limited. Future large multicenter studies are needed to address the specific correlates and risk factors of nocardiosis, and especially to investigate subgroups of patients with underlying diseases.
Selection bias of the control group was minimized by random sampling from the hospitalization registry. The control group in our study comprised hospitalized patients with pneumonia. It might be argued that this is not the optimal control group, and having healthy persons as controls is warranted. However, since nocardiosis is an opportunistic infection that mostly affects the lungs, our aim was to identify specific correlates of nocardiosis. The selection of healthy persons as controls could have resulted in identifying correlates of disease and hospitalization in general, or inflated measures of association. Therefore, patients with pneumonia were considered the most appropriate control group to address the study goal.
To our knowledge, this is the first study that assessed multiple correlates of nocardiosis. Corticosteroid therapy was strongly positively related to nocardiosis. The effect size was robust and varied amongst sub-populations; it was remarkably strong for pulmonary nocardiosis. Males and patients with chronic pulmonary diseases might be at a greater risk for nocardiosis when treated with corticosteroids. Our findings have clinical implications in the identification of patients at risk for nocardiosis and can guide clinicians' decision-making on immunomodulatory treatment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Coussement, J. et al. Nocardia infection in solid organ transplant recipients: A multicenter European case-control study. Clin. Infect. Dis. 63(3), 338–345 (2016).
Wang, H. L., Seo, Y. H., LaSala, P. R., Tarrand, J. J. & Han, X. Y. Nocardiosis in 132 patients with cancer. Am. J. Clin. Pathol. 142(4), 513–523 (2014).
Minero, M. V. et al. Nocardiosis at the turn of the century. Medicine (Baltimore) 88(4), 250–261 (2009).
Paige, E. K. & Spelman, D. Nocardiosis: 7-year experience at an Australian tertiary hospital. Intern Med J. 49(3), 373–379 (2019).
Martínez Tomás, R. et al. Pulmonary nocardiosis: risk factors and outcomes. Respirology 12(3), 394–400 (2007).
Steinbrink, J., Leavens, J., Kauffman, C. A. & Miceli, M. H. Manifestations and outcomes of Nocardia infections. Medicine (Baltimore) 97(40), e12436 (2018).
Beaman, B. L. & Beaman, L. Nocardia species: Host-parasite relationships. Clin. Microbiol. Rev. 7(2), 213–264 (1994).
Margalit, I. et al. Nocardia colonization in contrast to nocardiosis: A comparison of patients’ clinical characteristics. Eur. J. Clin. Microbiol. Infect. Dis. 39(4), 759–763 (2020).
World Health Organization. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (World Health Organization, Geneva, 1991).
Israel Central Bureau of Statistics. Characterization and Classification Of Geographical Units by the Socio-economic Level of the Population, 2013. https://www.cbs.gov.il/en/publications/Pages/2017/Characterization-and-Classification-of-Geographical-Units-by-the-Socio-Economic-Level-of-the-Population-2013.aspx (2017).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 40(5), 373–383 (1987).
Czock, D., Keller, F., Rasche, F. M. & Hussler, U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin. Pharmacokinet. 44(1), 61–98 (2005).
Greenland, S. Modeling and variable selection in epidemiologic analysis. Am. J. Public Health. 79(3), 340–349 (1989).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 57, 289–300 (1995).
Abramson, J. H. WINPEPI updated: Computer programs for epidemiologists, and their teaching potential. Epidemiol. Perspect. Innov. 8(1), 1 (2011).
Fatahi-Bafghi, M. Nocardiosis from 1888 to 2017. Microb. Pathog. 114, 369–384 (2018).
Rosen, L. B. et al. Nocardia-induced granulocyte macrophage colony-stimulating factor is neutralized by autoantibodies in disseminated/extrapulmonary nocardiosis. Clin. Infect. Dis. 60(7), 1017–1025 (2015).
Gramegna, A. et al. Atypical pathogens in hospitalized patients with community-acquired pneumonia: A worldwide perspective. BMC Infect. Dis. 18(1), 677 (2018).
Belchamber, K.B.R., Donnelly, L.E. Macrophage dysfunction in respiratory disease. Results and Problems in Cell Differentiation. 2017:299–313.
Dworski, R., Fitzgerald, G. A., Oates, J. A. & Sheller, J. R. Effect of oral prednisone on airway inflammatory mediators in atopic asthma. Am. J. Respir. Crit. Care Med. 149(4), 953–959 (1994).
Waljee, A. K. et al. Short term use of oral corticosteroids and related harms among adults in the United States: Population based cohort study. BMJ 357, j1415 (2017).
Dixon, W. G., Suissa, S. & Hudson, M. The association between systemic glucocorticoid therapy and the risk of infection in patients with rheumatoid arthritis: Systematic review and meta-analyses. Arthritis. Res. Ther. 13(4), R139 (2011).
Rosman, Y. et al. Nocardiosis: A 15-year experience in a tertiary medical center in Israel. Eur. J. Intern. Med. 24(6), 552–557 (2013).
Hardak, E., Yigla, M., Berger, G., Sprecher, H. & Oren, I. Clinical spectrum and outcome of Nocardia infection: Experience of 15-Year period from a single tertiary medical center. Am. J. Med. Sci. 343(4), 286–290 (2012).
Restrepo, A., Clark, N.M. Nocardia infections in solid organ transplantation: Guidelines from the Infectious Diseases Community of Practice of the American Society of Transplantation. Clin Transplant. March 2019:e13509.
Woodworth, M. H., Saullo, J. L., Lantos, P. M., Cox, G. M. & Stout, J. E. Increasing Nocardia incidence associated with bronchiectasis at a tertiary care center. Ann. Am. Thorac. Soc. 14(3), 347–354 (2017).
Haussaire, D. et al. Nocardiosis in the south of France over a 10-years period, 2004–2014. Int. J. Infect. Dis. 57, 13–20 (2017).
Sakyi, S. A. et al. Evaluating the contribution of Nocardia spp. and Mycobacterium tuberculosis to pulmonary infections among HIV and Non-HIV patients at the Komfo Anokye Teaching Hospital, Ghana. Can. J. Infect. Dis. Med. Microbiol. 2018, 2910198 (2018).
Peleg, A. Y. et al. Risk factors, clinical characteristics, and outcome of Nocardia infection in organ transplant recipients: A matched case-control study. Clin. Infect. Dis. 44(10), 1307–1314 (2007).
van der Laan, D. M. et al. Factors associated with antihypertensive medication non-adherence: A systematic review. J. Hum. Hypertens. 31(11), 687–694 (2017).
Ettenger, R. et al. Meeting report: FDA public meeting on patient-focused drug development and medication adherence in solid organ transplant patients. Am. J. Transplant. 18(3), 564–573 (2018).
Naganuma, M., Kunisaki, R., Yoshimura, N., Takeuchi, Y. & Watanabe, M. A prospective analysis of the incidence of and risk factors for opportunistic infections in patients with inflammatory bowel disease. J. Gastroenterol. 48(5), 595–600 (2013).
Redondo-Benito, A. et al. Opportunistic infections in patients with idiopathic inflammatory myopathies. Int. J. Rheum. Dis. 21(2), 487–496 (2018).
Cheng, T. et al. Systemic corticosteroid for COPD exacerbations, whether the higher dose is better? A meta-analysis of randomized controlled trials. Clin. Respir. J. 7(4), 305–318 (2013).
O’Donnell, A. E. Medical management of bronchiectasis. J Thorac Dis. 10(S28), S3428–S3435 (2018).
Calverley, P. M. et al. Determinants of exacerbation risk in patients with COPD in the TIOSPIR study. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 3391–3405 (2017).
McDonnell, M. J. et al. Comorbidities and the risk of mortality in patients with bronchiectasis: An international multicentre cohort study. Lancet Respir. Med. 4(12), 969–979 (2016).
Acknowledgements
This work was performed in partial fulfillment of the MPH thesis requirements of the Sackler Faculty of Medicine, Tel Aviv University. The authors would like to thank Ms. Cindy Cohen for her help with language editing and to Mr. Ashraf Morsi for his help with graphic design.
Author information
Authors and Affiliations
Contributions
I.M. conceived the research idea. I.M., K.M., E.G., and I.K. designed the research. I.M., Y.BA., and Y.S. collected the data. H.BZ. collected the laboratory data. I.M. E.G., and K.M. supervised all aspects of the study and analyzed the data. I.M wrote the initial draft. All authors contributed the interpretation of the results and to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Margalit, I., Goldberg, E., Ben Ari, Y. et al. Clinical correlates of nocardiosis. Sci Rep 10, 14272 (2020). https://doi.org/10.1038/s41598-020-71214-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71214-4
This article is cited by
-
Disseminated nocardiosis and anti-GM-CSF antibodies
European Journal of Clinical Microbiology & Infectious Diseases (2024)
-
Co-infection with Mycobacterium tuberculosis and Nocardia farcinica in a COPD patient: a case report
BMC Pulmonary Medicine (2023)
-
Molecular detection of Nocardia: development and application of a real-time PCR assay in sputum and bronchoalveolar lavage fluid samples
European Journal of Clinical Microbiology & Infectious Diseases (2023)
-
The Role of 18-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography (FDG-PET/CT) in Management of Nocardiosis: A Retrospective Study and Review of the Literature
Infectious Diseases and Therapy (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.